Keratoconus Treatment
All the support you need for your Keratoconus Treatment
Dr Geoffrey Ryan is a highly experienced eye surgeon with advanced training and experience across various eye conditions and treatments, and Keratoconus is no different. You’ll feel well-supported in your treatment journey with simplified explanations and care from Dr Ryan.


Are you struggling with Keratoconus?
If you’re struggling with blurred vision or constantly changing prescriptions, you may be experiencing keratoconus. Whatever the cause, we understand how frustrating this can be. Contact us today to discuss your options and find the right treatment for you.
Symptoms of Keratoconus
Blurred vision and light sensitivity are common symptoms of keratoconus, typically emerging during puberty or the late teens. These issues occur when the cornea weakens and changes into a cone shape. Other common symptoms include:
- Blurry or distorted vision
- Astigmatism and double vision
- Difficulty seeing in low light
- Nearsightedness
- Light sensitivity or vision loss
- Fleischer ring (discolouration around the eye’s front)
If you’re experiencing any of these symptoms, it’s recommended that you schedule an appointment with a keratoconus specialist. Early diagnosis and treatment can help manage symptoms more effectively and improve long-term eye health. Dr. Ryan is able to thoroughly evaluate your condition and discuss the best options for your care.


What causes keratoconus?
The cause of keratoconus is still being studied, but it is widely believed to result from a combination of genetic and environmental factors. Research by the Lions Eye Institute has found that around 1 in 10 people with keratoconus have a parent who also has the condition. It has also been found to be associated with:
- Eye rubbing
- Conditions including eczema, hayfever, allergies, Downs syndrome and Ehlers-Danlos syndromes
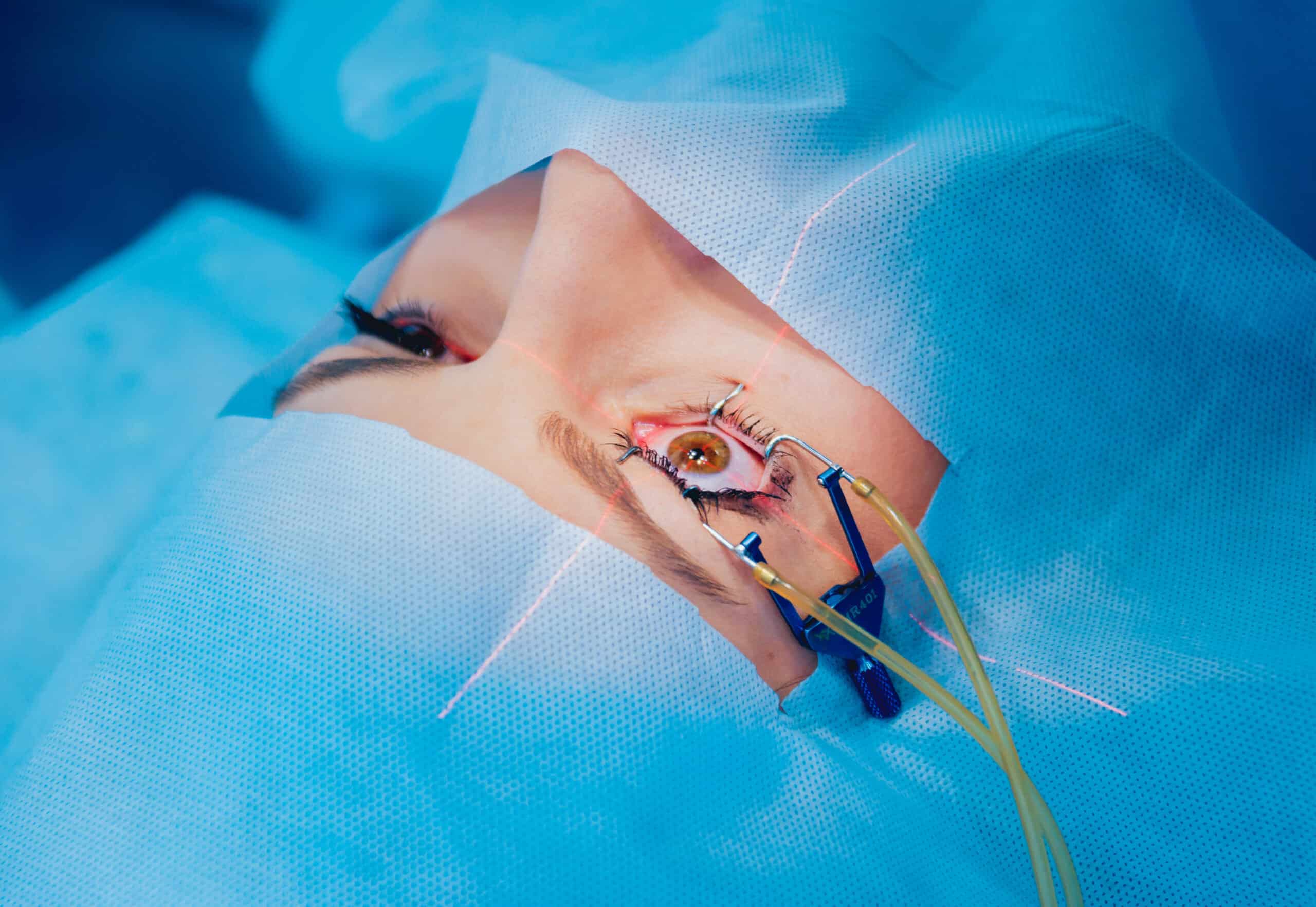
The Corneal Cross-linking Procedure
Dr Ryan is a corneal specialist who has a special interest in the treatment of Keratoconus. Corneal Cross-Linking is a modern procedure that combines riboflavin, oxygen and UV light to strengthen the collagen of the cornea.
Dr Ryan performs the “Boost Protocol” form of the procedure. It’s the very latest form of cross-linking. It offers you the advantage of avoiding the removal of the top layer (epithelium) of the cornea as the treatment is performed. This results in less pain and decreases the risk of infection, which can often come with older cross-linking protocols.
We use world-leading equipment
Consulting and treating eye conditions such as keratoconus from the Queensland Eye Institute, we’re fortunate to have access to the very best equipment for diagnosis and treatment. You’ll feel like you’re in safe hands with the quality of the clinic, experienced keratoconus specialists and advanced equipment.
Why trust Dr Ryan with your Keratoconus Surgery?
Advanced training Keratoconus treatment
Dr Ryan is an expert in Keratoconus and has advanced training in the treatment of this condition, including Corneal Cross-Linking.
The latest treatment options
The Queensland Eye Institute and Dr Ryan prioritise advancement in this area. We offer the latest in treatment options including “Boost Protocol” Corneal Cross-Linking.
A focus on less invasive treatments through disease prevention
Your quality of life, comfort, and future prognosis are important to us. We have a focus on preventing disease progression, which results in less invasive treatments.
State-of-the-art equipment
Consulting and treating keratoconus out of the Queensland Eye Institute, we have state of the art diagnostic and treatment technology available to us.
You’ll understand your procedure
Dr Ryan will always take the time to explain your procedure to you in plain language so you can understand what your condition means and what will happen during your procedure.
Important things to know
Don’t worry — you don’t have to remember all of this. You will be provided with a detailed handout with all the aftercare information following your surgery.
You’ll be educated on the key steps of preventing disease progression by Dr Ryan
If you are undergoing Corneal Cross-Linking Treatment, you’ll need to take three days off from work or study to recover.
A contact lens is placed on the eye for your comfort following the procedure. This is removed in the clinic a few days following your treatment.
What other treatments are available for Keratoconus?
Contact Lenses for the treatment of Keratoconus
Soft contact lenses are made of a flexible, water-containing material that conforms to the shape of the cornea. While they may be comfortable and easy to wear for many people, they are generally not recommended for patients with keratoconus. This is because the shape of the cornea in keratoconus is irregular and often too steep to be corrected with soft contact lenses. Soft lenses can conform to the shape of the cornea, but they can also conform to irregularities, resulting in poor visual clarity and discomfort.
In contrast, rigid gas permeable (RGP) lenses and scleral lenses are designed to provide a more uniform surface for the cornea, allowing light to focus properly on the retina and improving visual clarity. These lenses are made of a firm material that holds its shape and can help to correct the irregular shape of the cornea in keratoconus. Therefore, for patients with keratoconus, special types of contact lenses, such as RGP or scleral lenses, are recommended.
Corneal Transplant for the treatment of Keratoconus
In some severe cases of keratoconus, corneal transplantation may be the recommended treatment option. A corneal transplant involves replacing the damaged cornea with a healthy cornea from a donor. Typically, corneal transplants are successful in restoring vision and can drastically improve the quality of life for patients who have advanced keratoconus.
Like any surgery, though, this procedure does come with some risks. It is worth discussing your condition, its severity, and the potential treatment options with your surgeon. Recovery time for a corneal transplant can be lengthy, with follow-up appointments for the following months and special care required to ensure healing.
What’s the difference between a corneal transplant and a corneal collagen cross-linking procedure?
A corneal transplant, also referred to as keratoplasty, involves removing the damaged cornea and replacing it with a healthy donor cornea. This surgical procedure is typically recommended for advanced cases of keratoconus or when other treatments have not successfully improved the patient’s vision.
On the other hand, corneal crosslinking (CXL) is a non-surgical procedure that involves applying riboflavin drops to the cornea and then exposing it to ultraviolet light. This strengthens the collagen fibres in the cornea, which helps stabilise the cornea and prevent any further thinning and bulging.
CXL is typically recommended for early to moderate cases of keratoconus and can be effective for slowing or stopping the progression of the condition. Recovery from CXL is generally quicker than a corneal transplant, and most patients are able to return to normal activities in just a few days.
It’s important to note that while both procedures can be effective treatments for keratoconus, they are not interchangeable and are typically recommended for different stages of the condition.

Choosing the right Keratoconus specialist
When choosing a keratoconus specialist, consider their experience with the condition, expertise in the latest treatments, and ability to offer personalised care. Look for a specialist who provides comprehensive diagnostic tools, a clear treatment plan, and a supportive approach to managing the condition.
Dr Ryan is an experienced specialist in diagnosing and treating keratoconus. With extensive knowledge of the latest advancements in eye care, he offers customised treatment plans to help manage the condition effectively and achieve the best possible results.
Our Keratoconus FAQs
Keratoconus is a progressive condition, characterised by the thinning and bulging of the cornea (the front window of the eye), into the shape of a cone. The condition’s onset typically starts in early adolescence and progresses into the mid-20s and 30s.
We do not know what causes keratoconus. The condition may be inherited and is seen more often in people who are atopic (prone to allergies such as asthma or eczema). There may also be a link between people who vigorously rub their eyes and keratoconus.
In the early stages of keratoconus, most patients note a constantly changing glasses prescription. This is due to the progressive change in the shape of the cornea. Once the shape of the cornea becomes irregular, contact lenses will be required rather than glasses. In advanced cases, the cornea may develop scarring, resulting in a significant reduction in vision.
In the early stages, some patients will simply need glasses to see well, but many patients eventually require contact lenses to achieve better vision. The contact lenses are usually small, hard lenses (rigid gas-permeable lenses). Contact lenses do not make keratoconus better or worse; they just improve your vision when you wear them.
In advanced cases, where contact lenses fail to improve vision, a corneal transplant—or a ‘graft’—may be needed. However, most patients with keratoconus will not need a corneal transplant.
“Boost Protocol” Corneal Cross-Linking (CXL) is a new treatment that halts the progression of the disease. It is only required in patients who demonstrate ongoing changes in the shape of the cornea. It uses ultraviolet light and vitamin B2 (riboflavin) drops to stiffen and strengthen the cornea. This procedure is effective in over 90% of patients.
Keratoconus Blog Posts
A higher standard of care for eye conditions.
Book your appointment below or call our eye centre to schedule your consultation. Our friendly team is happy to answer any questions you may have.
Or call us on (07) 3239 5000



